“I find that the act of offering the option of an assisted death is one of the most therapeutic things we do,” Stefanie Green tells me. She sees it in the faces of her patients — they’re “relieved.” Sometimes it actually means they’ll choose to live longer, to keep fighting, because now they know they can end their suffering if it becomes intolerable.
I wanted to know if Green, a physician specializing in euthanasia in British Columbia, is finding her job easier now than she did at first. “Is it more normal for me to be writing scripts and picking up lethal drugs and driving across town and doing this?” she asks back. It’s a rhetorical question. “Yeah, it’s oddly okay for me to be doing that. I don’t find it shocking anymore, but the events are still extraordinary.”
Green has her own term for these extraordinary events, drawing on her prior experience as an obstetrician, when she helped bring people into the world. “At both ‘deliveries,’ as I call them, I am invited into a most intimate moment in people’s lives,” she writes in her book.
The procedure, she assures me on our call, is “100 percent effective.” If her patient asks to die, and if her schedule, her ethics, and the law permits it, she will administer a lethal injection.
Since Canada legalized euthanasia in 2016, there has been a strange balancing act at the heart of its medical system. There is a national suicide prevention hotline you can call 24/7, where sympathetic operators will try to talk you out of killing yourself. But today there are also euthanasia hotlines, where operators will give you the resources you need to carry out your wish. Doctors and nurse practitioners are now in the business of saving the lives of some patients while providing death to others.
Canada calls it Medical Assistance in Dying, or MAID. The term encompasses both assisted suicide, which is when providers give patients the means to end their own lives, and euthanasia, which is when a medical practitioner directly administers a patient’s lethal injection. But virtually all such deaths — over 99 percent — are euthanasia.
Supporters insist that this is not state-sanctioned suicide. Rather, it’s a dignified solution for those who no longer wish to suffer from terminal or chronic illness. MAID allows “for compassionate action, while also protecting those who are particularly vulnerable,” claimed David Lametti, the attorney general and minister of justice, in 2021.
Prime Minister Justin Trudeau has long promised to strike just this balance. In 2019, while pressing the need to expand access to euthanasia, he assured that people will be able to choose assisted death “in a way that isn’t because you’re not getting the supports and cares that you actually need.”
This is the promise of medical assistance in dying: that vulnerable people who want to die for the wrong reasons will be encouraged to live, as they always have been — while people who want to die for the right reasons will have their autonomous decision upheld. If even a single vulnerable person were pushed into assisted death, it would be a scandal to the system. That is why safeguards were put into place.
And yet stories describing just this — a system that does encourage the vulnerable to seek medical death — are coming fast and hard lately. A number of recent news articles have reported on Canadians who, driven by poverty and a lack of access to adequate health care, housing, and social services, have turned to the country’s euthanasia system. In multiple cases, veterans requesting help from Veterans Affairs Canada — at least one asked for PTSD treatment, another for a ramp for her wheelchair — were asked by case workers if they would like to apply for euthanasia.

As this article will show, in internal meetings, those close to the system have long talked openly about red flags that many people are choosing euthanasia because they’re not getting the “supports and cares” they need. The physicians in charge of the process not only know that this is happening, but they have discussed it in seminars, collected evidence, and then kept it quiet in public.
The safeguards promised by Trudeau and others to prevent vulnerable people from heading down the road to euthanasia turn out to be vague, pro forma, and easy to get around by doctor-shopping. And interviews with patients and their loved ones show that some of them, perhaps many, are making it to the end of that road.
One of the greatest reasons for concern is the sheer scale of Canada’s euthanasia regime. California provides a useful point of comparison: It legalized medically assisted death the same year as Canada, 2016, and it has about the same population, just under forty million. In 2021 in California, 486 people died using the state’s assisted suicide program. In Canada in the same year, 10,064 people used MAID to die.
Important people — prominent politicians, physicians, and judges — promised Canadians that their rights to autonomy would be expanded. But the picture that emerges is not a new flowering of autonomy but the hum of an efficient engine of death.
By the time I spoke to her, Stefanie Green had performed more than three hundred MAID procedures, making her among the most prolific providers in Canada. Her last one was just weeks before I talked to her.
Green was hesitant to speak with me at first. She is busy, and her services are in demand. But more than that, she doesn’t want to add any fuel to “unfounded opposition arguments,” as she put it by email. Her line of work already invites controversy.
But there’s no reason that it should, Green insists. Asked on a call about stories of abuse, she raises her voice and says, “you cannot access MAID in this country because you can’t get housing. That is clickbait. These stories have not been reported fully.”
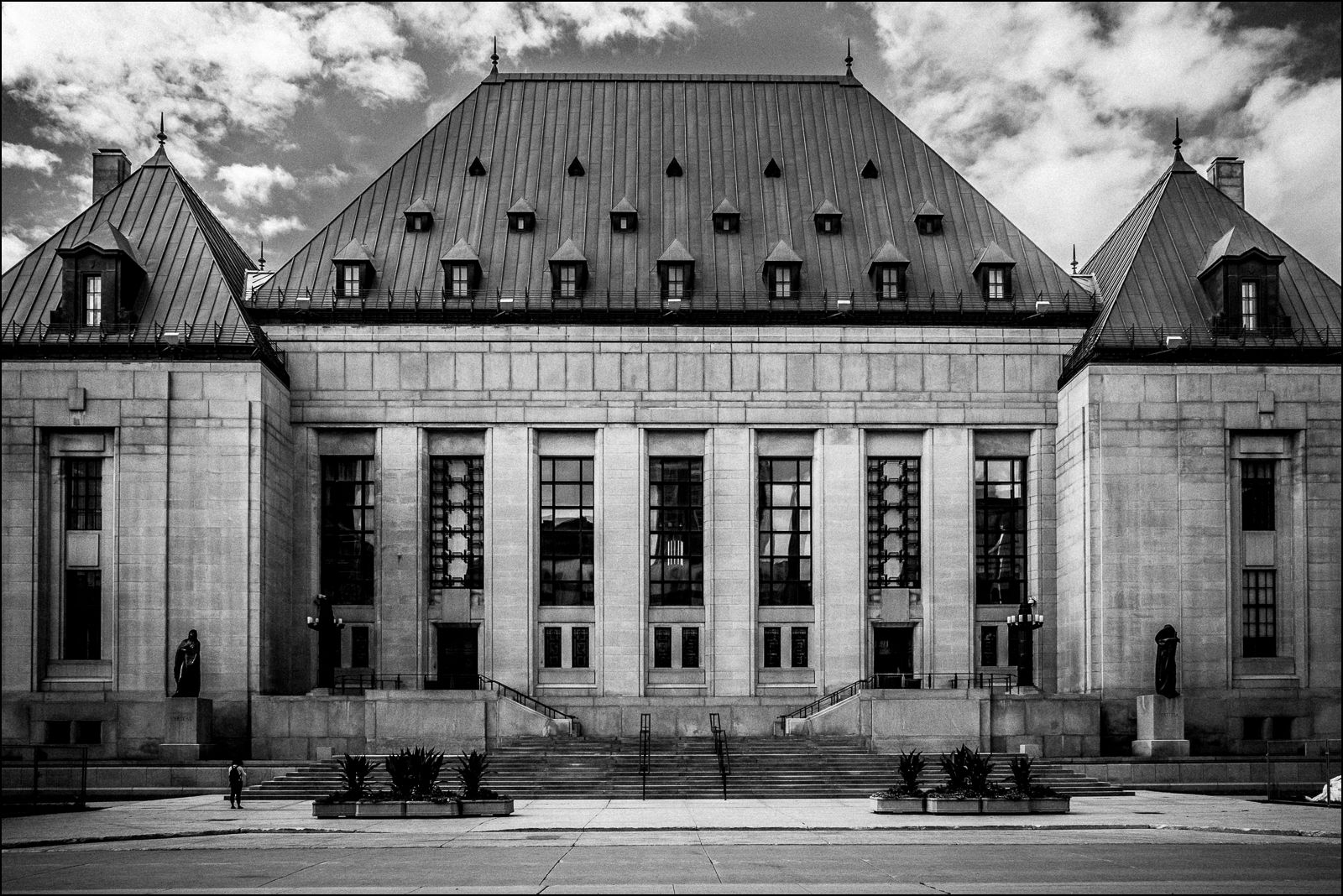
Green is echoing what from the beginning has been a refrain of euthanasia advocacy. In its ruling decriminalizing the practice, the Supreme Court of Canada echoed it too, asserting that “a permissive regime with properly designed and administered safeguards” would be “capable of protecting vulnerable people from abuse and error.” And the Canadian Broadcasting Corporation in 2017 assured its readers that it is a “misconception” that “MAID puts vulnerable people at risk.”
And advocates today insist that the safeguards are working. “We have four or five years of experience now, and absolutely no indications, that I’m aware of, of alleged misuse or poor decisions,” said James Cowan in 2021. Cowan is a former senator who helped lead the passage of the original legislation. Helen Long, the CEO of Dying with Dignity Canada, offered this line in a May 2022 Maclean’s essay, arguing that the stories that people “who are not able to access supports like safe and affordable housing are opting to have MAID instead” are “simply not true and there is no evidence that I’m aware of to support those claims.”
Yet even some euthanasia providers have expressed worry. In October, Madeline Li, a psychiatrist involved in drafting a national euthanasia training curriculum, testified to a parliamentary committee that the legislated safeguards are “impotent.” She added, “I believe the Canadian populace and maybe even the legislators are not aware of who has been qualifying for MAID.”
In fact, the evidence of abuse is there if advocates want to find it. The Canadian Association of MAID Assessors and Providers, the leading organization of Canadian euthanasia providers, has sat on credible evidence by its own members that people are being driven to euthanasia by credit card debt, poor housing, and difficulties getting medical care. These are people who do have some sort of medical condition but in many cases are using these conditions to check a box in the approval process, when the relief they are mainly seeking is from other forms of suffering. And the system is doing much more to help them down the path toward death than to protect them as the public was promised.
In addition to performing euthanasia procedures herself, Stefanie Green is president and co-founder of the organization, also known as CAMAP. It is not a government entity, but Green also stresses that it “is not an advocacy movement.” Instead, she says, it exists to fill “an absolute void” of interpreting federal law to clinicians. The organization’s website says it aims “to establish training resources, to create medical standards, and to encourage the standardization of care across the country.” And filling the void it is: In July 2022, Health Canada, the agency that is responsible for national health care policies, announced a plan to outsource its voluntary euthanasia training standards to CAMAP.
The organization regularly holds virtual seminars aimed at training euthanasia assessors and providers. The New Atlantis has obtained video recordings of several seminars held from 2020 through 2022, along with slideshows and material used by the presenters.
One seminar was specifically devoted to how to handle euthanasia requests from poor patients. In one recorded seminar, held on May 5, 2021, the first speaker is Kevin Reel, a senior ethicist at Sunnybrook Hospital and former president of the Canadian Bioethics Society.
Reel talks as if it’s a given that inadequate resources will drive people to request euthanasia — but he also sees a silver lining. He says that after decriminalization, “my first thought as an OT [occupational therapist] back then was, this could be an extraordinary lever to improve social supports in this country.” He continues, “if we can gather the stories of people who would opt to die, because the social supports are so poor — ,” and trails off. He says he wants to get a financial grant to get this project going.
But, Reel warns at a different point, individual MAID providers do not have the power to fix the problems with social supports that are driving patients to euthanasia: “you simply cannot fix the system.”
So while they wait for that distant day when society does solve poverty, how should MAID providers handle these cases?
Some providers are quite explicit about their answer. In response to “concerns voiced, that for some people, it is easier to access medical assistance in dying than to get the treatments they need to control symptoms,” several CAMAP members conducted a 2022 study in which they interviewed twenty euthanasia providers about their experiences. One provider responds:
I think we live in a society where we have structural inequities. And that really sucks…. But it doesn’t mean that we should be sheltering people from the option of having an assisted death. I think we keep seeing death, and MAID in particular, as the wrong outcome. And … that’s not my choice or my decision to make for someone.
Several of the seminars actually advise providers on how to handle the “moral distress” they will experience in such cases. Reel’s is one of them. “What I cannot do is remove all that moral distress from this work,” he begins. But “I can minimize it, help you minimize it and manage it through some tools that we’ll talk about.” Reel talks around and around this, evasively and emptily, never specifying why euthanizing poor patients might be morally distressing.
For another seminar speaker, euthanasia requests from poor people are just part of the job. Althea Gibb-Carsley recently retired as a care coordinator and social worker of Vancouver Coastal Health’s assisted dying program. The title of her presentation asks, “What is the role of the MAID assessor when resources are inadequate?”
She describes several cases that she managed as a care coordinator.
Take Mary, 55, who Gibb-Carsley says is “bright, creative, tenacious, determined” — “a dynamite person.” Mary has worsening fibromyalgia and chronic fatigue, both non-terminal medical conditions. (Gibb-Carsley doesn’t specify whether she is using real names or not.) Mary knows that she could control her pain if she could take vitamin pills, eat a special diet, and go to physiotherapy. She can’t afford it. “Mary identifies poverty as the driver of her MAID request,” Gibb-Carsley writes on a slide accompanying her talk, emphasizing the. “She does not want to die, but she’s suffering terribly and she’s been maxing out her credit cards. She has no other options.”
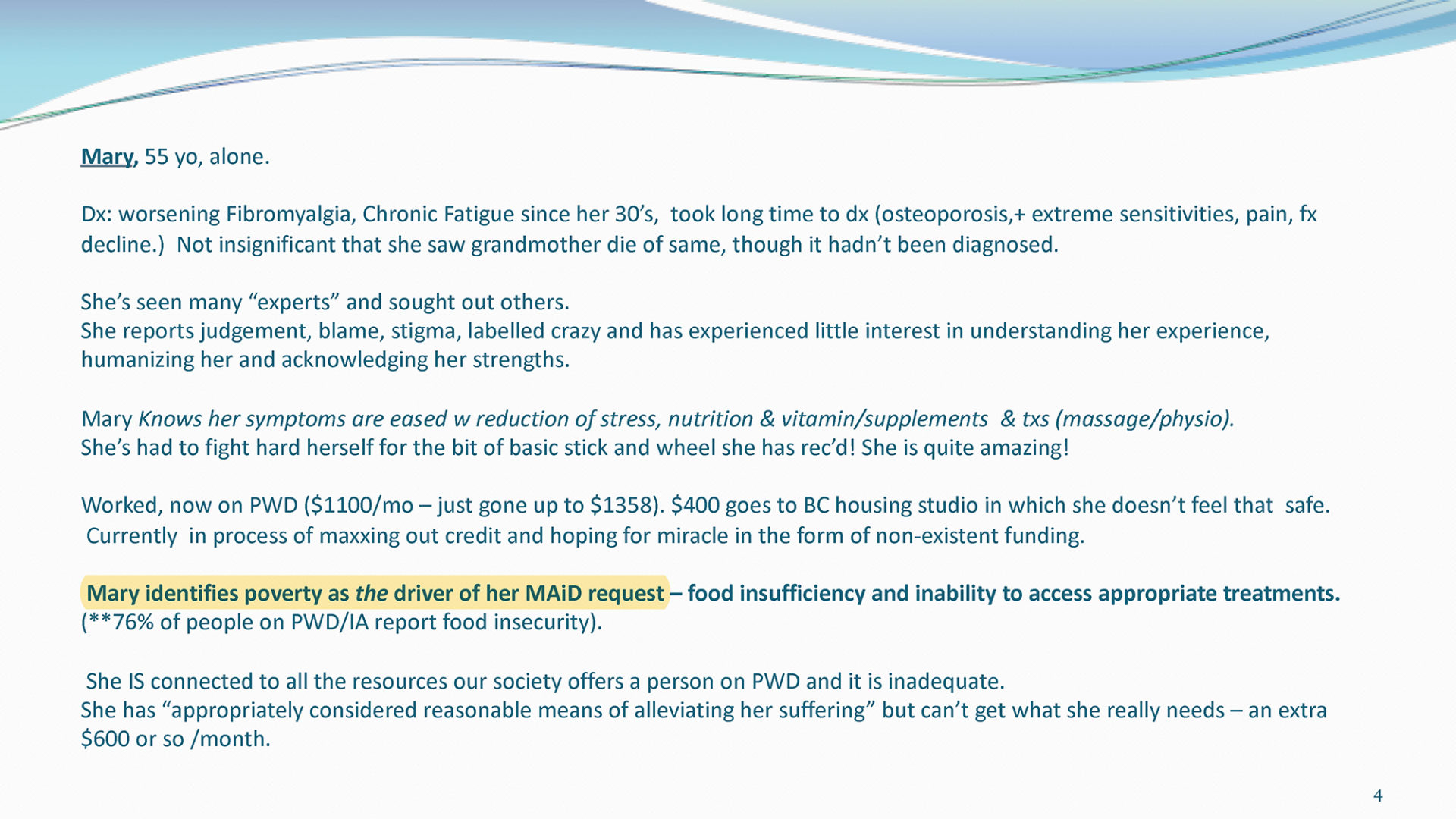
Then there is Nancy, 68, a former physician: “bright, capable, she’s tired, very, very tired.” Following a car accident, Nancy now has chronic pain. “She believed she had a lot more years to work,” so she didn’t save enough money. And there is Greg, 57, a writer who has diabetes, cardiac problems, anxiety and depression, and a history of trauma. Both need housing, but they can’t find any place that is accessible, safe, and affordable on an income mostly from disability benefits. The end is predictable. “Nancy has no other options,” while Greg’s “plan was to stretch his credit to the edges and then set a final date.”
Lucy, a 38-year-old trans woman, is an immigrant who has pain, osteoarthritis, depression, and anxiety. Although Lucy is “clever” and her college program is funded, it’s hard for her to concentrate on studies, and “people are so judgey.” She lives in a new one-room studio that has “no air or light and creepy men all around.”
Lucy was waiting for the law to expand to allow euthanasia not only for terminal illness, but for any “grievous and irremediable” condition. It is a vague standard, and some reporting suggests it could include osteoarthritis, the only diagnosed physical condition Lucy is described as having. We do not hear what happened to Lucy, but the expanded eligibility standard she was waiting on did take effect in 2021.
Gibb-Carsley says that these patients have “no other options” because of their poverty, their housing situations, their difficulty getting medical care. “I think you will find, and you know already,” she says to her audience of euthanasia providers, that if you want to offer your patients some alternative to MAID, “this will often mean a referral to not very much, and certainly not very fast.” It’s not that they are terminally ill or truly beyond help, but that they can’t get the help they need in the system right now, so euthanasia seems like the only way out.
Justin Trudeau made a clear promise to the public: that nobody would receive MAID “because you’re not getting the supports and cares that you actually need.” But the CAMAP recordings plainly suggest that exactly this is happening, that euthanasia workers know it, and that they are acting with no urgency to stop it.
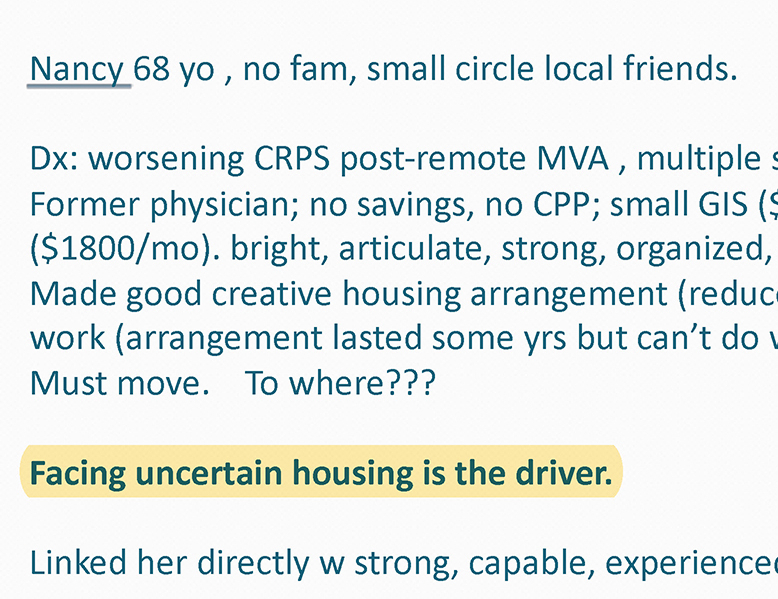
And just as important as what we hear on the recordings is what we don’t. Of Mary, the patient who identified “poverty as the driver of her MAID request,” we do not hear that the system discouraged and denied her application. Of Greg, who the slides say “identified housing as [a] driver” of his euthanasia request, we hear that he is “getting very close to needing to set a date” to be euthanized — and again, not that any effort is being made to stop him. Of Nancy, for whom “uncertain housing is the driver,” we hear of no effort to stop her.
In effect, though it’s not clear whether she recognizes it, Gibb-Carsley is an internal whistleblower. She is speaking directly to the organization whose mission is to guide Canada’s euthanasia practice. She is an expert the organization considered credible enough to invite to its internal meeting. And she is telling them that exactly the kind of abuse the system promised to prevent seems to be happening, perhaps often.
Consider a different case: The reason that camp counselors are told never to be alone with a child is not just to avoid actual abuse but to avoid the kind of situation in which doubts arise over whether or not abuse could occur. A system that protects against abuse is one that methodically identifies these situations, and, when they do happen, treats them as big red flags. It warns others about them and reforms the system to help prevent them. If the MAID system were working as promised, the presenters should be warning attendees that they must be vigilantly on the lookout for just the kinds of cases described in the seminar, scrupulously ensuring that they are not approved for euthanasia.
Instead, what we hear from Canada’s euthanasia professionals is vacillation, equivocation, delay, and excuses.
During the Q&A, no one in the seminar doubts that the stories are true. Nobody suggests strengthening the safeguards, alerting the public, or halting the system while the problem is worked out. Less than a decade into Canada’s experiment in medicalized death, with over 31,500 people dead, the speakers feebly propose to start collecting data.
Exhausted by science and tech debates that go nowhere?
The presenters clearly understand that what they are describing is a terrible moral problem. “Our silence is our complicity,” Gibb-Carsley writes on her last slide in a large font. But Gibb-Carsley and Kevin Reel do not present euthanasia driven by poverty as a problem for MAID. Actually, they suggest, it presents an opportunity to highlight the real problem: the inadequacy of the welfare state.
It’s as if the situation offers a silver lining. Reel excitedly talks about the problem as an “extraordinary lever” to lobby for improved welfare. Gibb-Carsley’s slideshow concludes, “trust in the evolution of this field of practice,” meaning the practice of euthanasia. “Your Assessments provide a rare opportunity to hear from the typically disenfranchised patients about their experiences.” The subtext of this sunny euphemism is that giving a voice to the voiceless will, for many, ultimately mean killing them.
The attendees understand too what they are hearing. “Given the vulnerability of patients who are maybe requesting MAID because of socioeconomic reasons,” one asks, “do you save yourself that moral and ethical distress by withdrawing?” Reel responds: “If withdrawing is about protecting your conscience, you have [an] absolute right to do so.” But he adds: “You’ll then have to refer the person on to somebody else, who may hopefully fulfill the request in the end.”
Justin Trudeau promised that the euthanasia system would not lead anyone to choose to end his or her life due to a lack of social support. But in private, even practitioners say that the support that Canada most efficiently provides to many vulnerable patients now is death.
Kevin Reel declined a request to comment on his recorded statements. Stefanie Green, president of CAMAP, was asked more than two days before this article went to press how she reconciles the seminar recordings with her earlier claim that stories of abuse are “clickbait” that “have not been reported fully.” Green requested and was provided information on how to access the recordings discussed in this article, but she did not offer comment.
How is all this happening?
A core reason that Canada’s assisted dying program has grown so much faster than any other program in the world is that it is the most permissive. Eligibility criteria began loose and are rapidly getting looser. You do not need to be terminally ill, only to have a “grievous and irremediable” condition, a standard that is open to significant differences in interpretation. In March 2023, mental illness alone will qualify as an acceptable medical reason to die. And the Quebec College of Physicians now suggests that Parliament expand euthanasia eligibility to minors and even newborns.
Despite all this, the MAID system was also supposed to be “carefully-designed” with “stringent limits” to prevent abuse. That was the charge put to the government by the Supreme Court of Canada in its 2015 ruling decriminalizing the practice. The court affirmed that “a permissive regime with properly designed and administered safeguards” would be “capable of protecting vulnerable people from abuse and error.”
But under such broad, permissive criteria for eligibility, the safeguards that were actually put into place are clearly not working.
Recognizing the need for guidance, CAMAP developed generalized assessment forms. Many doctors now use these to evaluate whether a person is eligible for MAID. I sent them to Paul S. Appelbaum, a professor of psychiatry, medicine, and law at Columbia University in New York City. Appelbaum, a leader in his field, has been practicing for four decades. In 1998, he helped develop a now widely used test for assessing whether patients are mentally competent to make medical decisions. In 2022 an expert panel convened by the Canadian government recommended his competency test to euthanasia assessors, an indication that Appelbaum’s authority is recognized by the MAID system itself.
“All in all,” says Appelbaum by email, “it doesn’t strike me as a particularly well-thought-through evaluation process.” Among other things, “it’s not clear from these forms how an evaluator would decide that a condition is ‘grievous and irremediable,’” he says, quoting one of the key legal criteria.
Moreover, the initial screening questions for depression and anxiety “are not detailed enough to result in a diagnosis, and even if they did, the impact the answers to these questions are supposed to have on the final decision about authorizing MAID is unspoken.” This matters because another key criterion is that patients be mentally competent to request their own deaths. What Appelbaum is saying here is that a person who may be depressed and suicidal — who ought to be helped to find hope, not encouraged to die — cannot properly be identified with these forms.
I also sent the CAMAP forms to Mark Komrad, a clinical psychiatrist and ethicist who helped craft the American Psychiatric Association’s statement against euthanasia for patients who are not terminally ill. His response was a single line: “Death by checklist!”
Part of what Komrad means is that the checklists are a tool available to MAID assessors, rather than a safeguard imposed upon them — they are not set by federal law. So in practice, the law leaves a great deal of latitude to euthanasia providers to decide whether the requirements are met.

For example, when I asked Stefanie Green how she decides whether a patient with a mental health condition has the competence to choose euthanasia, she said that she makes a judgment call about whether a patient has an “active” or “stable” case of mental illness. For “active” cases, she will consult a specialist; for “stable” cases, she proceeds on her own. Green is not a psychiatrist, so I asked Appelbaum about her framework. “It’s not a distinction that makes any sense to me,” he says.
This is a problem not only for Green. Under federal law, any physician or nurse practitioner can assess a patient and provide euthanasia, and in many provinces they can do so without any additional required training.
Now recall that in just a few months, mental illness will become a legal reason to receive MAID.
[Editor’s Note: On December 15, 2022, the day before this article was published, two Canadian cabinet members, including Minister of Justice David Lametti, announced that the government was considering delaying, but not canceling, the mental illness expansion. They stated that the move was not due to concern over existing safeguards, which “are excellent.”]
Then there is the problem of doctor-shopping.
What if a doctor dutifully screens for eligibility, and rejects someone? Then the person can just go elsewhere.
In another CAMAP seminar recording, we learn of a man who was rejected for MAID because, as assessors found, he did not have a serious illness or the “capacity to make informed decisions about his own personal health.” One assessor concluded “it is very clear that he does not qualify.” But Dying with Dignity Canada connected him with Ellen Wiebe (pronounced “weeb”), a prominent euthanasia provider and advocate in Vancouver. She assessed him virtually, found him eligible, and found a second assessor to agree. “And he flew all by himself to Vancouver,” she said. “I picked him up at the airport, um, brought him to my clinic and provided for him,” meaning she euthanized him.
Even doctors can doctor-shop. There is one final procedural safeguard: a second assessment by a clinician that agrees with the first. In practice, it’s nearly impossible to not meet this requirement. Jocelyn Downie, a prominent law professor who was part of the legal team that won the court case decriminalizing euthanasia, tells assessors and providers during a seminar that “you can ask as many clinicians as you want or need,” seemingly implying that you can do so until there is a concurring opinion. “Disagreement doesn’t mean you must stop,” she says in another seminar.
MAID assessments are highly subjective. We hear as much from the presenters in the CAMAP training seminars. Some physicians believe that advanced age should help qualify a person. Others don’t. In one session, a presenter says that providers “have a lot of different ideas” about how to assess whether someone suffering from Alzheimer’s has the capacity to choose euthanasia. It’s as if there are as many views of rational suicide as there are assessors. “There is no certainty or unanimity required. There is not perfection required,” says Downie. The result: There are many paths available to reach the end, and you only need to find one. The system makes it easy to die. (Asked by email how she would reconcile her statements in the seminars with the safeguard reassurances that have been offered to the public, Downie responded, “This is an inaccurate characterization of what I said and did at the two seminars.” She did not specify the nature of the inaccuracy.)
And even if the safeguards were more rigorous, they wouldn’t do much good, because the enforcement has been lax. Criminal investigations of MAID providers are exceedingly rare, and CTV News reported in 2022 that “federal officials don’t keep statistics on when such cases are reported to police.” Nancy Hansen, the Director of the Disability Studies program at the University of Manitoba, told me that in effect “there’s no consequences for non-compliance” with the law.
And that’s because the people doing the training, the assessments, the procedure, and informing the review are all the same people. These are the people, as Ellen Wiebe says often in her public speaking, for whom this is “the most rewarding work we’ve ever done.”
Wiebe declined requests to be interviewed for this article. Asked for comment about her statements in the seminar, she responded: “It is rare for assessors to have patients who have unmet needs, but it does happen. Usually these unmet needs are around loneliness and poverty. As all Canadians have rights to an assisted death, people who are lonely or poor also have those rights.”
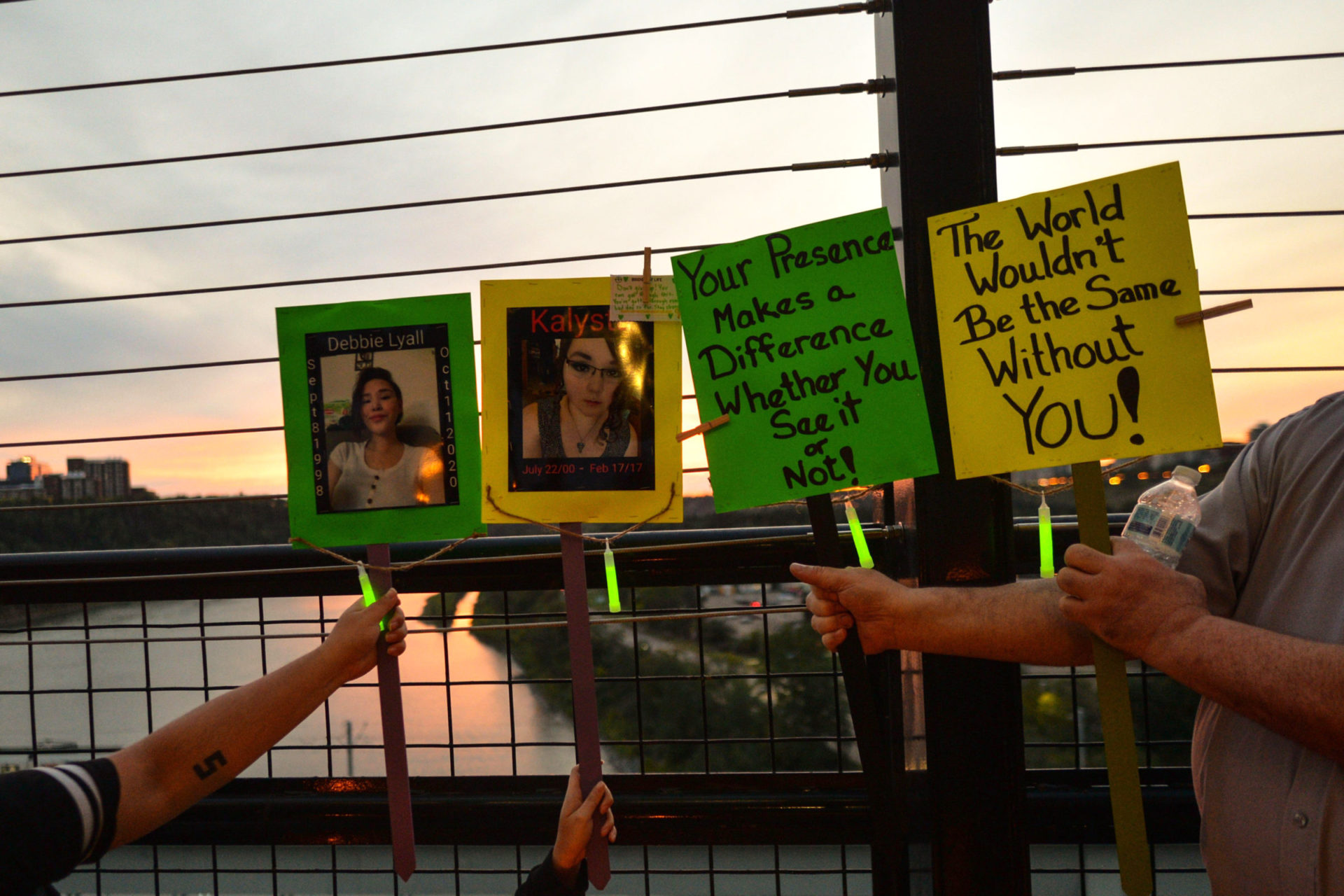
The clearest evidence that Canada’s euthanasia regime is failing to protect the vulnerable is the stories of patients themselves. They have spoken in a series of articles published in other outlets over the past year. They speak on social media. Some of them spoke to me for this article, as did the friends and confidants of another who is no longer with us to speak for herself.
The picture that emerges from them is of people who are in desperate circumstances and unable to get help, and are presented with an easy way out: to make it all go away through a medically assisted death.
Les Landry is in trouble. Why? Because he had the temerity to turn 65.
“I cannot afford to live,” he tells me over the phone from Medicine Hat, a small city in Alberta. “What do I do?” Even now he is thinking of solutions. He could move into his van or skip meals. He already stopped taking some of his prescriptions. But, he says, “MAID is the only choice I can see for a way out.” It just makes financial sense.

Les is surprised to find himself in this situation. He used to work as a truck driver, earning $85,000 a year. He married and had children. Then he got sick, developing an allergy to anesthesia during a routine hernia operation in 2009. His reaction was so severe that, for most patients, it would have been fatal. But he survived, and today, while he suffers from chronic medical problems, his death is no longer imminent — except with creative accounting.
For many years, Les got by with payments from Alberta’s disability welfare system. His fixed income was $1,820 a month, about 1,300 U.S. dollars. It was a modest sum, but “I was regularly comfortable.” More importantly, his benefits included a specialized diet, a service dog, prescriptions, and modest travel for medical appointments. He was told it would be for life.
But Les just recently turned 65, the age at which his pension begins and all those disability benefits end. The result, he says, was a significant net loss of income. He no longer has the critical support he needs.
Les is a fighter. “Even at 65, I don’t want to die,” he says. He says it again and again. “I really don’t want to die. I just can’t afford to live.” Les knows that he could end his life already, if he wanted to. He feels forgotten; he feels pushed to end his life. He doesn’t need a government service to do that. “I have enough medication already to kill a horse,” he says. “The only thing that MAID does is to make my suicide socially acceptable.”
When Les emailed a MAID team to apply, he wrote, “I turned 65 [and] lost all m[y] disabilities benefits and now a senior in poverty. I am not going to live my life like this.” On December 2, Les received his first approval for euthanasia. He is now waiting for the second and final approval. And he says he will doctor-shop until he gets it.

When Rosina Kamis decided that she could not take any more, she wrote up a list of reasons why she needed to be “euthanized ASAP.” If all you knew about Rosina were her medical history, you could be excused for assuming that MAID was meant for someone like her. At 41 years old, she was in constant pain from her fibromyalgia, had chronic leukemia and a myriad of other mental and physical illnesses, a long list of medications, and a rotating cast of attending physicians and nurses. This is also what she told her assessors: that she had no quality of life, was confined to her bed, and in constant pain.
But that is just one presentation of her story. Rosina was not dying: in ordinary circumstances her medical conditions were chronic, not terminal. And a wealth of material reviewed for this article — interviews I conducted with her friends and powers of attorney, emails she sent to her powers of attorney, emails to herself and to her physicians, emails to her abusive ex-husband, her Google Drive, a recording of her second MAID assessment, recordings of her doctor appointments, recordings of calls trying to get pain control, videos she posted to a tiny group of YouTube followers, and medical documents — paint a much messier picture than what she showed her assessors.
Oftentimes, Rosina was hungry. The artificial light in her room would make her migraines worse. It was loneliness driving her to MAID, that she “must suffer alone” with her service dog — which she could “easily lose,” as her landlord was trying to evict her and she had nowhere else to go. It was that she didn’t want her physicians to harm her by changing her pain medication, as they sometimes did. It was that she was “scared” of being institutionalized; that what she needed to live was not what she could reasonably expect to get; and that others would benefit from her death because MAID “is the best solution for all.” Her choices seemed slim. When her fingers hurt, she couldn’t make food. She would post a video of herself going to bed, in her dark room, hungry and crying.
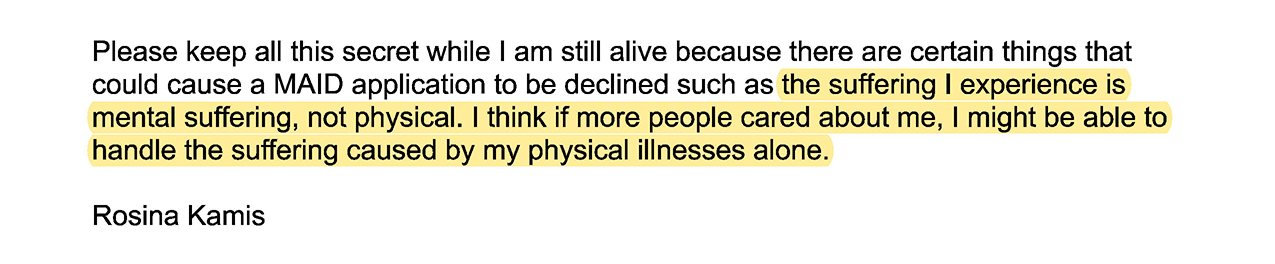
Rosina showed one face of her suffering to the MAID system, and another to her confidants. To the latter, the reasons she gave for really wanting to die were not physical suffering. “Please keep all this secret while I am still alive because … the suffering I experience is mental suffering, not physical,” Rosina wrote in a message apparently intended for her powers of attorney. “I think if more people cared about me, I might be able to handle the suffering caused by my physical illnesses alone.” To her two dozen subscribers on YouTube, she said, “Sometimes all the pain will go away just by having another human being here.”
She also saw herself as a burden. On a GoFundMe page that Rosina started to help buy food, she wrote, “Whenever I try very hard to get my needs met, I am seen as being manipulative…. I know I am hurting other people simply for having special needs. So, I have decided that the best thing for me and everyone else on this planet is for me to obtain Medical Assistance in Dying.”
In a recording she made of her assessment, which happened over the phone, the assessor tells her, “I just wanted to reassure you that with MAID it is a very dignified death. Rosini,” — the assessor gets her name wrong — “it is. There’s nothing embarrassing about it. You don’t lose control of your bowels. It’s a very elegant, graceful, dignified death.”
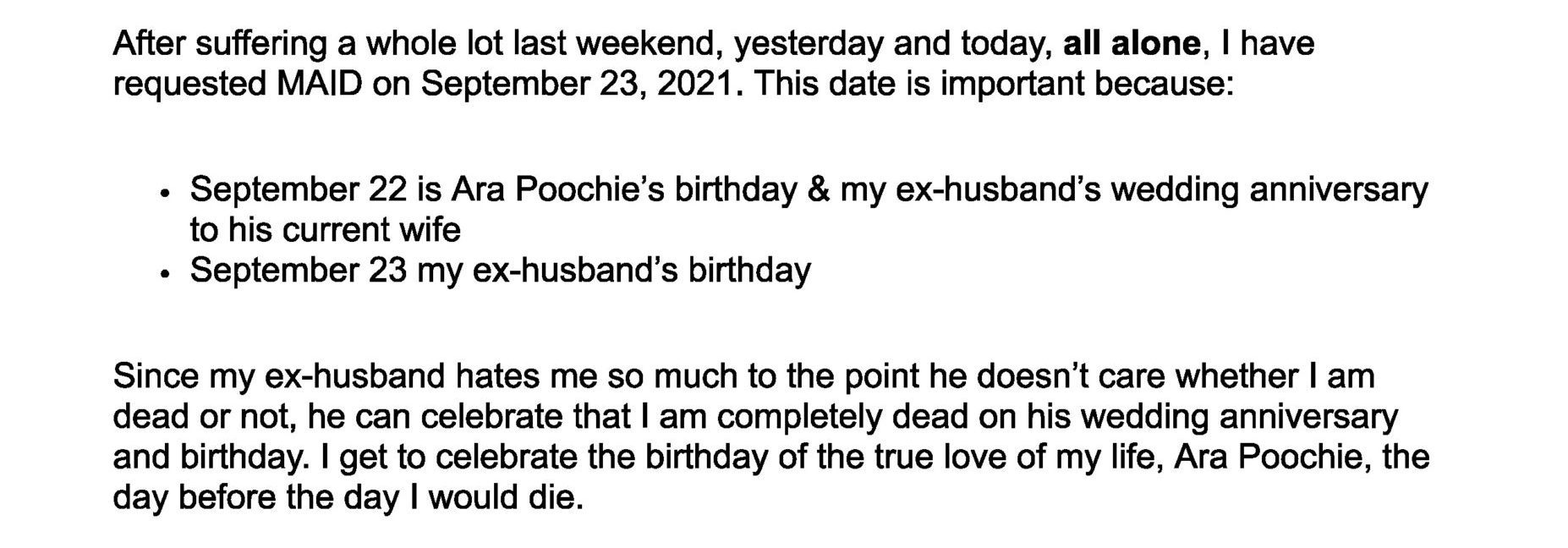
Rosina was approved, and specifically asked to die on the date of her ex-husband’s birthday. Rosina died in her shared basement apartment on September 26, 2021, after a doctor gave her a lethal injection.
Whatever your view on euthanasia, stories like Les’s and Rosina’s are not entirely straightforward. In many cases it is hard to sort out the tangle of internal and external reasons someone might make a voluntary request to die. But that is precisely the problem. Canadians were promised a system that would distinguish a rational choice to die from a desperate cry for help. But in stories like Les’s, Rosina’s, and so many others, that distinction breaks down.
This is particularly true in cases where a patient seeking euthanasia has a history of depression. As the psychiatrist Paul Appelbaum told me: “People with depression can be extremely rational in explaining the reasons for the decisions that they’re making. And what is most difficult is to separate the effect of the depression on that decision from what their underlying non-depressed motivations might be.”
We see this problem in the dramatic changes in Rosina’s stated reasons for wanting to die, and in the fact that she had been diagnosed with major depressive disorder. And we see it in the fact that Les has a history of suicidality.
There is a hard question, then, of what to do in ambiguous cases. Should we hold patients’ autonomy as sacrosanct when they say they want to die — and shrug them off as unreliable when they say they really want to live?
Canadian law requires that a qualifying medical condition for MAID be “incurable” and “irremediable.” But providers already have ample evidence that their patients’ conditions might be remedied if they could access better resources and medical care.
According to an internal study of MAID assessments, presented to CAMAP in 2022, of 54 patients who were not terminally ill, two-thirds had concurrent mental illness. A fifth of the patients had difficulty finding “appropriate” treatment. And, most disturbingly, over a third of patients were “not offered appropriate / available treatments.”
While many euthanasia providers pay lip service to saving those who can still be helped, others are more frank. Take Ellen Wiebe, the poster child for Canadian medical death — in 2016 Maclean’s covered her as a visionary. She has since become one of the most prolific MAID providers, having personally euthanized over 400 patients. In testimony to a parliamentary committee, Wiebe said that she would consider a patient on a five-year waitlist for an effective treatment to have “irremediable suffering.”
Elsewhere, in a public talk, Wiebe described a recent procedure she performed, saying, “It was a beautiful death.” And she admitted that the real difficulty is not protecting the vulnerable from abuse: “Angry family members are our greatest risk,” she says, and laughs.
Based on vague criteria and with precious little oversight, the MAID system has given enormous latitude to euthanasia providers to make the judgment calls about who should be helped to live and who should be helped to die. The result is a system that is highly efficient at finding reasons patients should qualify, not reasons they shouldn’t.
Althea Gibb-Carsley did not respond to requests to be interviewed for this article. But, asked for comment about her statements in the seminar, she replied: “The people I was aware of whose decisions to apply for MAID were influenced by their poverty, and a long-lived experience of lack of access to respectful and appropriate resources, also had medical diagnoses that meant they met the legal criteria for assisted death in Canada. Poverty and lack of resource[s] was not the reason they were found eligible for MAID.”
What this amounts to in practice is a very weak interpretation of the mandate to protect the vulnerable from abuse. We hear this in one of the CAMAP recordings, where, yes, Gibb-Carsley does tell her audience that people whose sole reason for requesting an assisted death is poverty should not be approved “in the absence of a chronic disease.” But, as she quickly acknowledges, “they often go together.”
Just so. For the poor and the vulnerable, for those who are “not getting the supports and cares” they need, as Justin Trudeau put it, all that doctors need to do is find some medical pretext to end their lives. Much as the man with a hammer comes to see everything as a nail, again and again Canada’s euthanasia system looks at vulnerable people and sees good candidates for medical death.

In December, an ad video by the Canadian fashion company La Maison Simons, titled “All Is Beauty,” went viral online. It told the story of Jennyfer Hatch, a 37-year-old-woman with Ehlers-Danlos syndrome who had chosen euthanasia. Slickly produced, the video showed slow-motion images of people gathered on beaches. At one point it describes “the most beautiful exit,” apparently referring to MAID. Hatch was euthanized the day before the campaign launched. She had told friends and interviewers that she wanted to live, but couldn’t afford it.
The tide has turned, and Canada’s vulnerable patients know it. They know how Canada’s system sees them. It shows up in how they see themselves, how they think about their choices.
Catherine Frazee, a disability scholar, told me by email about a doctor colleague who
has observed patients who become fixated on MAID, who under different circumstances, before MAID was a part of our culture, would have carried on living through difficult times, or who would have pursued treatment options with a reasonable chance of success even though doing so would be temporarily unpleasant or uncomfortable. Many people who are not at risk of suicide are nevertheless at risk of MAID, especially so because it has been so quickly embraced as an honourable, “dignified,” idyllic form of death.
You even hear this firsthand from some euthanasia providers — like Madeline Li, who told Parliament, “I’ve certainly had cases where I felt compelled to provide MAID against my better clinical judgment because the law did not adequately protect.” You hear it too from psychiatrists like John Maher, editor of the Journal of Ethics in Mental Health, who told Parliament that he has patients who could get better but “are now refusing effective treatment to make themselves eligible for MAID.”
Amy Hasbrouck, a disability advocate, told me that MAID is a way to “get rid of disabled people.” It’s an extreme view. Yet it is possible to imagine a euthanasia system that is set up without that intention, even one that is nominally set up to protect the vulnerable — and yet that, step by step, becomes indistinguishable from a system deliberately designed to usher them to their deaths.
From Rosina, Les, Mary, Nancy, Greg, Lucy, and so many others across Canada, what we hear are the cries of people in despair asking for help. Just a few years ago they would have been textbook candidates for what a just society would say: Your life has value. In Canada today they hear something else: Your death will be beautiful.
If you are in crisis or experiencing suicidal thoughts, help is available to you at:
• The National Suicide Prevention Lifeline in the U.S. at (800) 273-8255 or by dialing or sending a text to 988
• Talk Suicide in Canada at (833) 456-4566 or by text at 45645
• Crisis Text Line for mental health and violence crises via text, phone, web chat, and WhatsApp in the U.S., Canada, UK, and Ireland